PERIPHERAL FACIAL PALSY REHABILITATION MISTAKES TO AVOID
Professor Peggy Gatignol, Speech Therapist, Phd, Professor Tankéré’s department, Pitié Salpêtrière Hospital Group.
Peripheral facial palsy (PFP) is a common pathology that has an incidence of 14 to 25 / 100,000 inhabitants per year (Tankéré and Bernat, 2009). Even though 70% of cases will resolve completely, the remaining 30% will experience after-effects such as hemifacial spasms and synkinesis.
Peripheral facial palsy significantly impacts a patient’s quality of life. The repercussions, both physical and psychological, hinder their daily verbal and non-verbal communication. (Gatignol et al, 2011 ; Lannadère et al 2016)
I : PERIPHERAL FP ASSESSMENT AND REHABILITATION
Performing a standardised medical assessment (an MRI scan of the entire length of the facial nerve including the parotid) and rehabilitation are indispensable for the optimal implementation of a personalised rehabilitation programme. The goals of treatment are to meet the patient's needs, promote functional recovery, and to prevent and / or limit after-effects related to peripheral facial palsy. See chapter.
Obviously, and on the strength of our practice (400 patients per month), peripheral facial palsy which does not fully resolve within 1 month of onset will result in mild or significant after-effects. Rehabilitation begins early, within 15 days of the onset of facial palsy, regardless of the initial grade (Gatignol et al., 2011). It is based on massages and practical exercises aimed at promoting fibre recovery. Regular monitoring will make it possible to control, observe and adjust the various parameters related to movement.
II. REHABILITATION FOR PERIPHERAL FACIAL PALSY
The therapist will carefully consider the clinical context (sudden and / or progressive facial paralysis over several months), in particular the date of the examination compared to the date of paralysis onset. In addition, it is necessary to know the pathophysiology of the nerve damage. This is why it is important to have certain benchmarks. Indeed, after a parotidectomy, and with the preservation of the nerve, rehabilitation is not necessary because recovery takes place in 3 months and 15 days. After ear surgery or pontocerebellar angle (APC) surgery, the physical therapist will be the first to refer the patient for further investigations should the patient remains flaccid for more than 7 months after ear surgery and 10 months after APC surgery.
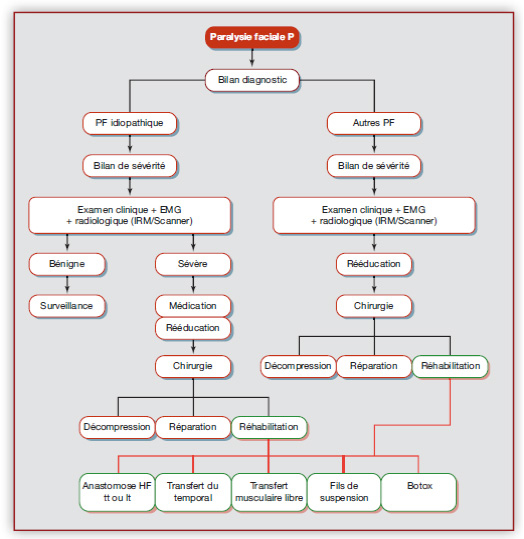
Diagram 1: Decision-making axes for the management of peripheral facial palsy
II.A THE IMPORTANCE OF SELF-REHABILITATION AND PATIENT INVESTMENT
Rehabilitation must be individual, personalised, and based on practical exercises which can be preceded by relaxation or massages. The use of electrical muscle stimulation has been banned since 1984. Diels, Gatignol, Mono.
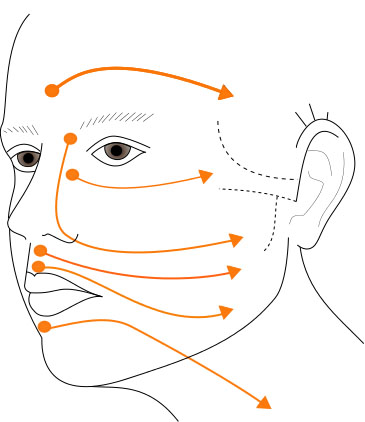
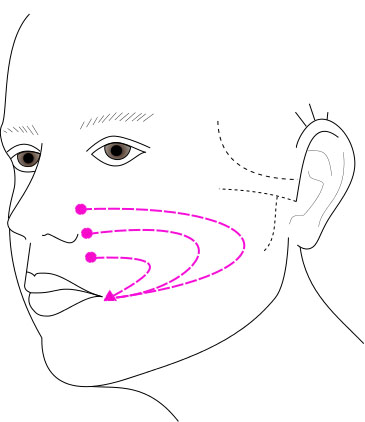
Secondly, the patient will be given advice on daily hygiene and harmful behaviours to avoid (eyelid protection using compresses, chewing gum, making faces) which can cause spasms and synkinesis. . The patient will then be taught massage techniques (sense, direction, intensity, duration) so that they can carry them out independently. He/she will then leave with a diagram illustrating the right moves to perform. See diagrams below in Diagrams 2a and 2b.
II.B MANUAL THERAPY
Massages aim to prevent contractures and the appearance of permanent after-effects. At the sequelae stage, massages aim to reduce hypertonia by loosening fibrous tissue adhesions. This is done by breaking down the fibres to stop contractures and relax the paralysed hemiface as much as possible. After applying a neutral cream, the patient massages the paralysed side of the face once a day for 10 to 15 minutes (to prevent hypertonia and synkinesis) and also the healthy side of the face (to help them avoid overly favouring this side).
External massages are performed from the centre to the periphery of the face in a symmetrical manner and should always remain parallel to the ground below. Massages are performed from the upper to the lower area of the face, 3 to 5 times per movement. They must be firm in nature (a pressure of 4 on a 5-point scale) and follow the direction of the muscle fibres. This indicates the direction of reinnervation to the nerve
All these massages (27 episodes) are now available on our YouTube channel: facial palsy pitié salpêtrière.
Intra- or endo-oral massages are performed with a thumb-index finger pinch (the thumb inside the cheek and the index finger on the outside). They aim to treat after-effects, notably spasms and contractures, using a stretching technique, whereby concentric stretches are carried out to lift up painful points. Once the contracture is located, we aim to make it disappear by stripping the fibres through repeated stretching. It is important to note that the appearance of these painful contractures indicates the start of reinnervation, in that they represent the often-inevitable beginnings of recovery of facial mobility with sequelae. (Lannadère et al, 2016).
The Neuromuscular Retraining (NMR) therapy we carry out aims to restore facial symmetry and facial expressions. (Diels, 2000). This programme is based on 3 main principles:
- The slowness of movements which allows the patient to modify the appearance, strength, and speed of execution. This helps increase motor control and prevent synkinesis.
- Small movements which limit the hyperactivity of neighbouring muscles.
- Symmetry of movements which reinforce the normal physiological response and limit hyperactivity on the healthy side.
Practical exercises are organised in several stages. Respecting these stages is essential because it helps to avoid co-contractions or even spasms. Picard et al, 2020b.
Chronological stages of traditional care
| Passive Stage | > | The patient visualises the movement. The therapist performs the movement for the patient. In the event of some movement by the patient, the Passive-Assisted stage will be recommended. |
| Passive-Assisted Stage | > | The patient looks at their reflection in a mirror and tries to initiate the movement. When the therapist detects a tremor, he accompanies the motion and maintains it for a few seconds in order to stimulate the patient's visual and cognitive attention. |
| Active-Assisted Stage | > | The therapist only maintains the gesture at the end of the movement. |
| Active Stage | > | When the motion is sufficient to trigger movement, the patient works alone in front of the mirror, without any forcing or exaggeration. |
| Active-Counter-Resistance Stage | > | When the patient manages to maintain the movement, the therapist applies slight resistance. |
Well-conducted NMR functional rehabilitation helps develop cortical control in facial expressions and rehabilitate a patient’s smile in communication situations. This principle is also the basis for palliative surgeries. Indeed, during surgical rehabilitation of the face, the tone of the face can be controlled by either a nerve or muscle. Whether it consists of a hypoglossal-facial nerve anastomosis (HFA) or a lengthening temporalis myoplasty (LTM), rehabilitation involves a process of motor, conscious and unconscious learning, involving the memory”. This neuroplasticity occurs during the work on facial expressions, particularly the smile, by modifying the organisation of the cortical zones via the feedback pathways.
Essential:
- A grade greater than II on the House and Brackmann classification scale, a total score of less than 85% on the Sunnybrook Facial Grading System at 3 months, and the commencement of treatment within 4 days of paralysis onset, seem to be prognostic factors for recovery with sequelae in the French-speaking population.
- No chewing gum, making faces or electrical stimulation.
- Pregnant women are 3.3 times more likely to develop idiopathic peripheral facial palsy; treatment remains the same.
- High dose corticosteroid therapy, an MRI scan and rehabilitation sessions should be prescribed.
- Synkinesis appears between the 4th and 7th month. (Picard et al, 2020b).
Bibliography:
1. Tankéré F., & Bernat I. Paralysie faciale a frigore : de l’étiologie virale à la réalité diagnostique. La Revue de médecine interne, 2009. 30(9), 769-775.
2. Lamas G. Réhabilitation de la face paralysée. Les monographies Amplifon, Eds 2016,n°60. En accès libre = https://www.amplifon.com/documents/406814/1006539/Monographie-Amplifon-num%C3%A9ro-60/ff6b6bf5-4fab-43fb-9567-38140c13b0c2
3. Gatignol P., Lannadère E., Bernat I., Tankéré F, Lamas G. Bénéfices de la rééducation d’une paralysie faciale périphérique. Revue Médicale Suisse, 2011, 7 1908-1913.
4. Lannadère, E., Picard, D., & Gatignol, P. Principes de rééducation d’une paralysie faciale périphérique. Les Monographies Amplifon, N°60, Eds 2016 (89-115).
5. Diels H.J. Facial paralysis: is there a role for a therapist? Facial Plastic Surgery, 2000, 16(4), 361-364
6. Picard, D., Lannadere, E., Robin, E., Hervochon, R., Lamas, G., Tankéré,F., Gatignol,P. (2020). Oro-facial motor assessment: validation of the MBLF protocol in facial palsy. Eur Arch Otorhinolaryngol. 2020 Jun 27.
7. Picard, D, Leroy R, Poussy T, Tankéré F, Gatignol P (2020b). Sequelae in bell's palsy: Prognostic factors for recovery. Ann Chir Plast Esthet. 2020 Oct 6:S0294-1260(20)30162-X.